Viruses and mutations
Natural selection has shaped the evolution of humans, plants and all living things on the planet. Though viruses aren't technically living they still need a host organism in order to reproduce. Therefore, they are subject to evolutionary pressures. Viruses mutate constantly particularly those which contain RNA as their genetic material such as coronaviruses and influenza viruses. All viruses are made up of a bundle of genetic material (either DNA or RNA) that's covered by a protective coating of proteins. Once a virus gets into the body mainly through the mouth and nose it latches onto our cells. The virus's DNA or RNA then enters the cell, where it can make copies of itself that go off and infect other cells. If the virus can copy itself and hijack enough of the person's cells without being wiped out by our immune system we get sick and become infected.
The human immune system uses numerous reactions to fight pathogens. The pathogen's job is to evade the immune system, create more copies of itself and spread to other hosts. Characteristics that help a virus do its job tend to be kept from one generation to another. Characteristics that make it difficult for the virus to spread to another host tend to be lost. Take, for example, a virus that has a mutation that makes it particularly deadly to its human host and kills the host within a few hours of infection. The virus needs a new, healthy host for its descendants to survive. If it kills its host before the host infects others, that mutation will disappear. One way hosts protect themselves from a virus is to develop antibodies to it. Antibodies lock onto the outer surface proteins of a virus and prevent it from entering host cells. A virus that appears different from other viruses that have infected the host has an advantage: the host has no pre-existing immunity, in the form of antibodies, to that virus. Many viral adaptations involve changes to the virus's outer surface.
Every now and then, an error occurs during the virus's copying process. That's a mutation. Mutations can either make the virus stronger or weaker, more infectious or less infectious. These mutations that are genetic mistakes are present when the virus replicates and will become passed on and eventually becomes part of the virus's normal gene. As these mutations accumulate over time we get new viruses strain variants. Therefore, it is important to bear in mind that virus strains variants emerge through the process of mutation. In the media sometimes the words strain and variant are often used interchangeably.

Mutations in SARS-CoV-2 virus
As SARS-CoV-2 spreads around the globe, it is mutating. There are two new coronavirus variants that have emerged recently. Each has its own set of mutations, but they both contain small changes to parts of the spike protein that helps the coronavirus attach to our cells. So far the main concern is that these new virus variants make the virus more easily passed from one person to another. Even though the main question is the impact of these new variants on the pandemic in reality there are numerous factors which contribute to how quickly a virus spreads, mainly via human behaviours including hand hygiene and social distancing, among others. But the variant that's become common in England is estimated to be more than 50% more contagious than earlier versions of the virus. The good news is that the variant strains being detected today still look very similar to the original strains that started the pandemic and were used to develop and test vaccines.
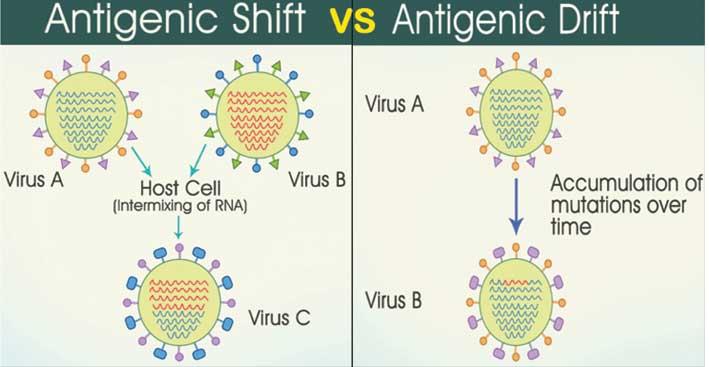
Much of our knowledge of how viruses change to escape natural or vaccine-elicited immunity comes from observing the influenza virus and constantly updating influenza vaccines. Influenza viruses change in two main ways, antigenic drift and antigenic shift. A comparison of the similarities and differences between coronaviruses and flu viruses may help us understand how those similarities and differences could impact potential Covid-19 vaccines.
Antigenic drift
As a virus replicates, its genes undergo random "copying errors" (that is genetic mutations). Over time, these genetic copying errors can, among other changes to the virus, lead to alterations in the virus' surface proteins or antigens. Our immune system uses these antigens to recognise and fight the virus. So, what happens if a virus mutates to evade our immune system? In influenza viruses, genetic mutations accumulate and cause its antigens to "drift", meaning the surface of the mutated virus looks different than the original virus. When the influenza virus drifts enough, vaccines against old strains of the virus and immunity from previous influenza virus infections no longer work against the new, drifted strains. A person then becomes vulnerable to the newer, mutated flu viruses. Antigenic drift is one of the main reasons why the flu vaccine must be reviewed and updated each year, to keep up with the influenza virus as it changes.
Is this also happening to the SARS-CoV-2?
It is being observed that SARS-CoV-2 virus is mutating relatively slowly as compared to other RNA viruses. In fact, studies to date estimate that the novel coronavirus mutates at a rate approximately four times slower than the influenza virus. It should be noted, however, that SARS-CoV-2 is a newly discovered virus infecting humans. There are still many unknowns and our understanding of the SARS-CoV-2 virus continues to grow. This relatively slow mutation rate for SARS-CoV-2 makes us hopeful that investigational SARS-CoV-2 vaccine candidates will potentially have one less hurdle toward offering the ability to provide protection over a longer period of time.

Antigenic shift
Influenza viruses undergo antigenic shift, an abrupt, major change in the virus's antigens that happens less frequently than antigenic drift. It occurs when two different, but related, influenza virus strains infect a host cell at the same time. Because influenza virus genomes are formed by eight separate pieces of RNA, sometimes these viruses can "mate" in a process called "reassortment". During reassortment, two influenza viruses' genome segments can combine to make a new strain of influenza virus. Reassortment results in a new subtype of virus, with antigens that are a mixture of the original strains. When a shift happens, most people have little or no immunity against the resulting new virus. Viruses emerging as a result of antigenic shift are the ones most likely to cause pandemics.
The coronavirus genome is made of a single, very long piece of RNA. However, when two coronaviruses infect the same cell, they can recombine, which is different than reassortment. In recombination, a new single RNA genome is stitched together from pieces of the two "parental" coronaviruses genomes. It's not as efficient as reassortment, but scientists believe that coronaviruses have recombined in nature. When this happens, scientists identify the resulting virus as a "novel coronavirus". The generation of a novel coronavirus, although occurring by a different mechanism than antigenic shift in influenza viruses, can have a similar consequence, with pandemic spread.
Alternatively, pandemic influenza viruses can sometimes arise, not by reassortment but by "zoonosis", when an influenza virus that infects other animals, often birds or pigs, makes the leap into humans and starts to spread. This happens with coronaviruses too, with new human coronaviruses or genes of new human coronaviruses, coming from ancestral coronaviruses that have infected other animals, such as bats, camels or pangolins. To date, we have seen coronaviruses act like influenza viruses in generating outbreaks and now a pandemic from processes of recombination and zoonosis generating novel human coronaviruses (resembling the antigenic shift and zoonotic origin of new human influenza virus subtypes). Thus far, we have seen human coronaviruses mutate but not undergo antigenic drift. This is good news for coronavirus vaccines. Nevertheless, given the similarities between the behaviour of influenza viruses and coronaviruses, there is ample reason to remain vigilant for the possibility of future antigenic changes in SARS-CoV-2 and to be prepared to alter a potential Covid-19 vaccine, if necessary.
Conclusion
In the end, the shape-shifting nature of the coronavirus (and all viruses) is something that experts across the world were expecting yet these new variants are not expected to change the course of the pandemic overnight. However, the contagiousness of the newer variants is all the more reason to remain vigilant and follow public health measures for preventing the spread of the virus - like wearing a mask, washing your hands, limiting close contact with others and getting vaccinated when you're able.
Rebecca Caruana is a Medical Student at the University of Malta