World AIDS Day, the day we commemorate and remember those lives we have lost to AIDS, the Acquired Immune Deficiency Syndrome which develops when HIV infection is left untreated. HIV is a sexually transmitted infection which can affect any person irrespective of gender, sexuality or occupation. Even though there are vulnerable groups who are at a higher risk of contracting and acquiring the virus (young women and girls, men who have sex with men, transgender people, sex workers and injecting drug users) one would be failing themselves and others if they think that they are immune to the virus.
Between January and September 2018, there have been 54 new HIV cases reported in Malta, an increase of 20% from the previous year. Meanwhile, countries with advanced HIV response like the UK, Australia, and France continue to report a decrease in the number of new diagnosis. It beggars belief that Malta being a tiny country with a population of around 500,000 people cannot introduce and implement strategies which effectively control the transmission of a sexually transmitted infection. Whilst the increase in number of new diagnosis could be attributed to an increase in the number of people accessing HIV testing services, the 6-8 weeks waiting list to get a sexual health screening at the GU clinic does not augur well for those who are attempting to access these services. A recent, educational, video on HIV self-testing by Allied Rainbow Services, an LGBT organisation in Malta, uploaded on Facebook showed how one could make use of an HIV test in the comfort of their own home. However, with a hefty price of €40, not many are in a position to purchase it. If the Government's resources to increase the staff and extend the opening hours of the GU clinic are stretched, it might want to consider subsidising the price of HIV self-testing kits.
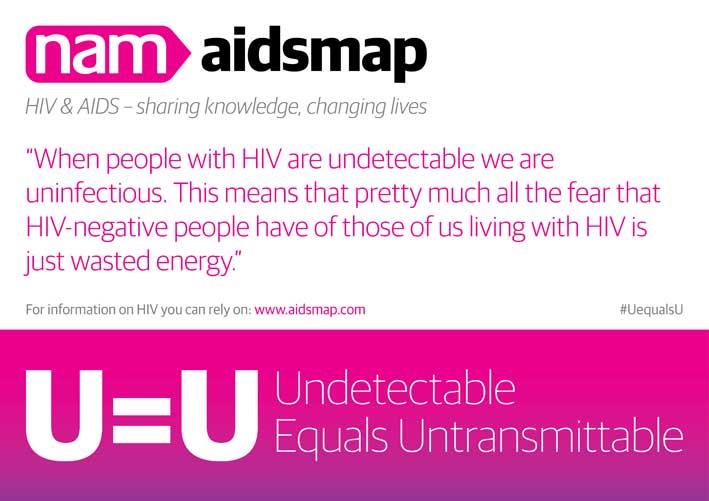
Undetectable = Untransmisttable (U=U)
It is now a scientifically proven fact that a person living with HIV who is on effective treatment and who has retained an undetectable viral load (lower than 200 copies/mL) for a period of 6 months cannot sexually transmit the virus to another person, even in the absence of condoms during sex. In other words, a person living with HIV can become non-infectious. With this in mind, one cannot simply emphasise enough the importance of the 'test and treat' approach. A person who gets a positive HIV diagnosis should be provided with Anti-Retroviral Treatment (ART) (the treatment given to people living with HIV) without any delay. It cannot be any treatment, however. The drugs which formed part of the early ART are known to have considerable, unpleasant side effects on the person taking them. Thankfully, the newer drugs have less side effects. People living with HIV had to, in the past, take up to 5-6 tablets a day to control the viral load (the number of copies of the virus in the blood). Nowadays, we find single-tablet regimens where the combination of two or more drugs required to suppress the virus are found in one tablet. This facilitates improved adherence and improves the quality of life of the person living with HIV. Unfortunately, in Malta not only are the single tablet regimens not available, but the ART prescribed is one which has been struck off international HIV guidelines. This to the detriment of people living with HIV whose quality of life is being put in jeopardy.
PrEP
PrEP, the single tablet which, taken daily or intermittently, can prevent the acquisition of HIV was unheard of until a couple of years ago. It is now celebrated as being one of the key tools to end the HIV epidemic. Its effectiveness has been reported in numerous studies and has been endorsed by international organisations including UNAIDS, WHO and CDC. It is therefore unbecoming that people living in Malta do not have access of PrEP on the NHS. One might argue: Why should I, from my taxes, pay for a pill which prevents acquisition of HIV? Why should not the people who are at higher risk fund it themselves? Cannot a person use a condom instead? There are several answers but the principle one rests on is that HIV is a threat to public health and governments have an obligation to keep infectious diseases at bay. Secondly, it is cheaper to provide PrEP than to provide ART, and thirdly, whilst condoms remain an effective tool to stop transmission of HIV and other STIs (PrEP only prevents the acquisition of HIV) we have, over the years, seen a decrease in condom use. Therefore, we have to, be proactive in the sexual health strategies and action plans we put into place.
LGBTIQ Action Plan
Last September, the government launched an 'LGBTIQ Action Plan' which also includes the updating of ART and also the introduction of PrEP. The inclusion of HIV within such an action plan takes away all the effort and hard work which HIV and LGBT+ activists have put in place in order to remove the stigma which HIV in the LGBT+ and non-LGBT+ community still carries. The government could argue, and rightly so, that in Malta the highest number of HIV cases are to be found in the MSM community. Nonetheless, internationally, more than 50% of the people living with HIV are women. The action plan is sending out the message that only those who identify as LGBT+ are at a high risk of acquiring HIV. One hopes that the government is still in time to take HIV out of the action plan and design an action plan which deals specifically with sexual health with particular focus on HIV which would fall under the Ministry of Health, and Education.
Matthew Hodson, the executive director of NAM - the HIV/AIDS information charity- writes on Twitter: "HIV is a virus. It is incapable of judgement; it does not moralise. HIV is not Santa Claus. It doesn't care if you've been bad or good." This is the message that we, as rational human beings, are expected to endorse. Stigma and discrimination, unfortunately, still persist around the world. Even though science has given us the tools we need to eradicate the virus, fighting people's regressive approach towards sexual health does not come easy. It cannot be treated with just a pill but only with a sound and comprehensive sexual health strategy which includes a holistic sexual health education, starting from secondary schools.
You can book a sexual health screening at the GU clinic (Mater Dei Hospital) by calling 2122 7981.
[email protected]
Dr Rapa is a lawyer who works as a Teaching and Research Assistant for the Masters in healthcare ethics and law at the University of Manchester. He is the founder of www.prepingmalta.com, a member of the European AIDS treatment Group (EATG) and EATG Training Academy Step-up programme Alumni 2017